Helpful Links
What is hypertension? |
Hypertension is the medical term for high blood pressure. It occurs most commonly in older cats with certain conditions like kidney and thyroid disease. Hypertension can be primary or secondary in nature. Hypertension can also be caused by “white coat syndrome” or the stress of the vet visit – this is one of the many reasons why our staff do not wear white coats or other identifying clothing!
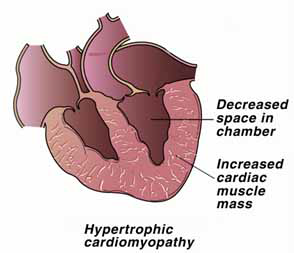
What causes hypertension?Primary hypertension has no identified underlying cause; it is much less common and is poorly understood. Secondary hypertension occurs as a result of an underlying disease process. Chronic kidney disease (CKD) and hyperthyroidism have been identified as the two most common predisposing factors for development of feline hypertension. In humans, hypertension is related to several factors, including a stressful lifestyle. Although not all causes of feline hypertension have been identified, stress does not appear to play a role in the development of this disorder in cats. · Kidney disease: It appears that several different mechanisms may lead to development of hypertension in cats with kidney disease. One theory suggests that as a cat ages, the kidneys undergo normal aging changes including a slow accumulation of scar tissue. With time, this scar tissue causes the kidneys to shrink in size. When the kidney shrinks, it is harder for the blood to filter through. Because the kidneys normally receive 20% of the blood with every heartbeat, blood backs up into the arteries and leads to an increase in blood pressure. One study found that about 60% of cats in old-age kidney failure have hypertension. Elderly cats in the early stages of kidney disease may also have hypertension. · Hyperthyroidism: The thyroid gland is located in the neck and plays a very important role in regulating the body's metabolic rate. Hyperthyroidism is a disorder characterized by the overproduction of thyroid hormone and a subsequent increase in the metabolic rate. This is a fairly common disease of older cats. Although the thyroid gland enlarges, it is usually a non-malignant change (benign). Less than 2% of hyperthyroid cases involve a malignant change in the gland. Many organs are affected by hyperthyroidism, including the heart. The heart is stimulated to pump faster and more forcefully, and eventually the heart enlarges to meet these increased demands for blood flow. The increased pumping pressure leads to a greater output of blood and high blood pressure. About 25% of cats with hyperthyroidism have high blood pressure. What are the clinical signs?Visual abnormalities are the most common clinical findings with feline hypertension. These abnormalities can include dilated pupils that do not constrict with light, blood within the chamber of the eye, and blindness. Blindness develops because high blood pressure in the eye causes the retina to detach. Other possible indications of high blood pressure include restlessness, agitation, decreased grooming, head pressing, changes in appetite, thirst and/or weight. Oftentimes, owners feel that their cats are more restless or agitated at night. These problems may be temporary or permanent, just like in people and only time can tell which ailments will resolve and which will be long lasting. Cats that do not feel well, just like people, may act in ways we would refer to as cranky, easily agitated, or aggressive towards people, especially children, and/or other animals. Why is hypertension bad?Left untreated, hypertension can lead to a number of negative side effects including: · Eye damage: hypertension can cause blindness due to damage of the retina from enlarged blood vessels · Brain damage: hypertension can lead to seizures, stroke, altered mentation, head tilt, and neurologic deficits · Kidney damage: damage to the tiny working parts of the kidney called the glomerulus can lead to further decreased kidney function as well as protein loss from the kidneys (proteinuria); proteinuria further damages the kidneys and can worsen kidney disease more quickly · Heart damage: hypertension causes increased workload for the heart, which can lead to the development of heart disease which can in turn cause arrhythmias, infarcts to the heart (think of a stroke, but instead of the brain the heart is affected), and heart failure How is it diagnosed?Hypertension should be suspected in any older cat with kidney disease or hyperthyroidism. Onset of sudden, unexplained blindness should raise a strong suspicion for hypertension, and the associated diseases should be considered, meaning that labwork to detect kidney and thyroid disease should be performed. Also, the presence of a heart murmur or kidney-related problems may signal the presence of a hypertensive state. Blood pressure is determined with a device that can detect blood flow in arteries. We use a pediatric blood pressure cuff in a manner very similar to the way human blood pressure is taken. We take the pressure on your cat’s leg. What is involved in treatment?The most commonly used drug is amlodipine (generic) which is Norvasc. Daily oral medication is required to control high blood pressure. This is not a cure. If you stop giving the medication as prescribed, the blood pressure can rise up into the abnormal and potentially dangerous high range again. The medication is a very small pill available at our office as well as any human pharmacy. This medication can be made into a liquid by an outside compounding pharmacy for those who find liquid easier to administer. Rechecking blood pressure once medication is started and then at regular intervals dictated by your veterinarian is extremely important. This is the only way to know whether or not the medication is working and if adjustments to the dose of medication are necessary. What is the prognosis?The underlying disease that caused hypertension to develop must be cured or controlled. Long-term success depends on whether or not this is possible. If the cat has kidney, heart, or thyroid disease, it is important to treat those conditions aggressively. These conditions are not curable (with the exception of one type of treatment for hyperthyroidism), so management of the disease is essential. However, even those can be managed successfully in most cats for many years, with excellent quality of life. If the cat has blindness due to detached retinas, a medical emergency exists. Blood pressure must be lowered quickly in order to regain vision. If the retinas remain detached for more than a day or two, the prognosis is poor for a return of normal vision. Therefore, the key to a successful outcome is rapid diagnosis and early administration of the proper medication to lower blood pressure. When controlled, hypertension has an excellent prognosis. Continued monitoring with blood and urine samples is important to rule out concurrent disease contributing to hypertension. |


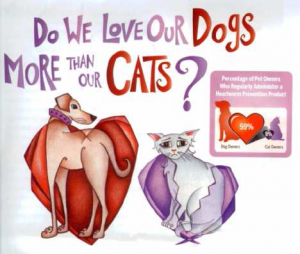 The good news is that heartworm infection is easy to protect against; the bad news is only 59% of dog owners and less than 5% of cat owners protect their pets by giving them a heartworm preventative! Considering that heartworm disease has been reported in all 50 states, these percentages mean that not all pets that are at risk of infection are protected.
The good news is that heartworm infection is easy to protect against; the bad news is only 59% of dog owners and less than 5% of cat owners protect their pets by giving them a heartworm preventative! Considering that heartworm disease has been reported in all 50 states, these percentages mean that not all pets that are at risk of infection are protected.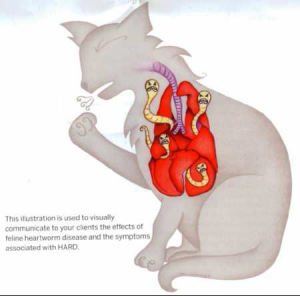 The signs of heartworm disease vary from pet to pet. Dogs may cough, have difficulty breathing and wear out quickly (referred to as exercise intolerance). In cats, the most common signs are coughing, difficulty breathing and vomiting, but they can also include blindness, convulsions, diarrhea, fainting, and loss of appetite or weight.
The signs of heartworm disease vary from pet to pet. Dogs may cough, have difficulty breathing and wear out quickly (referred to as exercise intolerance). In cats, the most common signs are coughing, difficulty breathing and vomiting, but they can also include blindness, convulsions, diarrhea, fainting, and loss of appetite or weight.

